Indoor air quality (IAQ) in hospitals is more than a matter of comfort, it’s critical to patient safety and infection control. From surgical suites requiring sterile conditions to isolation rooms designed to contain airborne pathogens, every zone within a healthcare facility must be closely monitored and regulated. Poor IAQ can delay patient recovery, increase the risk of airborne disease transmission, and compromise staff safety. Hospitals depend on precise environmental controls to address these risks, and they continuously monitor key factors such as temperature, humidity, carbon dioxide (CO₂), volatile organic compounds (VOCs), and air changes per hour (ACH).
Critical Parameters for Hospital IAQ
- Temperature and Humidity Control
- Pressure Monitoring & Differential Pressure Control
- CO₂, VOC, and Air Change Monitoring
-
Temperature and relative humidity affect not only patient comfort but also microbial growth and the performance of sensitive medical equipment. Maintaining strict control over these parameters is essential in areas like neonatal intensive care units (NICUs) and operating theaters. Instruments such as digital temperature and humidity sensors ensure stable conditions and help meet strict regulatory guidelines.
-
Maintaining proper room pressure differentials is vital to controlling pathogen transmission1. Hospitals use negative pressure in isolation or airborne infection isolation rooms (AIIRs) to prevent contaminated air from escaping, and positive pressure in operating theatres to block the ingress of external contaminants.
-
Carbon dioxide levels are a key indicator of ventilation efficiency and occupancy load. Excess CO₂ can signal inadequate fresh air exchange, which may allow airborne contaminants to accumulate. Meanwhile, VOCs — emitted by cleaning products, disinfectants, and building materials — can cause respiratory irritation and other health issues. Real-time gas sensors and IAQ monitors provide essential feedback to maintain safe levels.
Air changes per hour (ACH) is another vital metric, measuring how frequently indoor air is replaced. High-sterility areas like operating rooms require elevated ACH to maintain cleanliness, while isolation rooms demand customized ACH levels to ensure containment. Monitoring airflow rates helps facilities maintain compliance with CDC and ASHRAE standards.
Isolation and Operating Room Pressure Monitoring
Controlling pressure differentials between an isolation room and the anteroom (a small room located just outside the isolation room) is vital. Negative pressure isolation rooms are designed to effectively contain airborne infectious agents by ensuring that air flows into, but not out of, the room. Operating rooms, on the other hand, are maintained at a positive pressure to push clean air outward and keep contaminants at bay. Room Pressure Monitors and Differential Pressure Gauges play a critical role in continuously verifying these conditions and provide alerts when pressure deviates from safe thresholds, enabling rapid intervention.
The RSMC StabiliSENSE™ Critical Room Status Monitor enhances pressurization control in isolation rooms and operating suites by providing real-time monitoring and visual indication of room conditions. With a high-contrast touchscreen and customizable color-coded status alerts, staff can instantly verify whether rooms are maintaining required positive or negative pressure. Built-in audible and visual alarms notify personnel when conditions deviate from safe parameters, supporting immediate corrective action. Compatible with BACnet and Modbus® protocols, the RSMC integrates easily into existing building automation systems, ensuring continuous visibility and documentation of critical environmental conditions.
For healthcare environments that require multi-parameter monitoring beyond just room pressurization, the RSME Room Status Monitor offers advanced solutions. Designed specifically for critical spaces, it measures and displays differential pressure, temperature, and humidity on a sleek touchscreen interface, making it ideal for isolation rooms and surgical suites where comprehensive environmental oversight is essential. With built-in audible and visual alarms, the RSME ensures rapid response to deviations in any monitored parameter. Its native BACnet and Modbus® communication enables seamless integration with building automation systems, allowing facility managers to track trends, verify compliance, and maintain safe indoor air quality conditions across multiple zones.
For environments where mechanical reliability and zero‑power operation are essential (such as isolation anterooms, surgical support spaces, or temporary hospital wards) the Series 2000 Magnehelic® Differential Pressure Gauge offers an effective and reliable solution. This rugged, IP67-rated analog gauge requires no power or electronics, using a patented frictionless Magnehelic® mechanism to provide instant visual feedback on positive, negative, or differential pressure. Its shock‑ and vibration‑resistant die‑cast housing, precise ±2–4 % full-scale accuracy (±1 % available), and accessibility to zero‑adjustment without removing the cover ensure dependable long-term monitoring. Ideal as a fail-safe backup or standalone verification device, the Series 2000 reinforces pressurization protocols even during power outages or system interruptions, supporting safety and compliance in critical healthcare zones.
Indoor Environmental Monitoring Systems
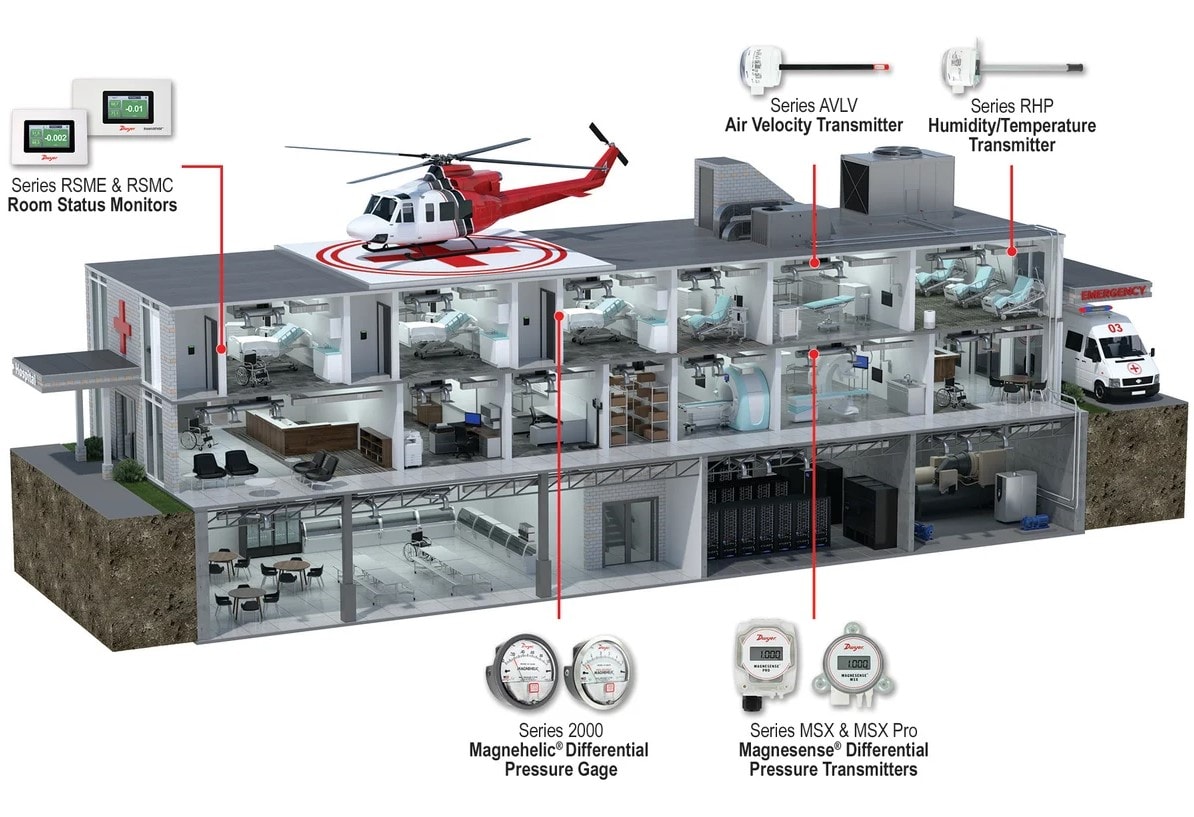
Modern hospitals use integrated IAQ monitoring systems that provide centralized oversight of environmental conditions. These systems combine data from multiple sensors to offer real-time visibility and automated control. They streamline facility management and ensure consistent performance by logging data and triggering alerts. Temperature Sensors and Humidity Sensors are used to ensure a comfortable environment for building occupants. These devices help ensure that proper temperature and humidity levels are maintained and assist in minimizing the spread of viruses/diseases and preventing mold growth.
The RHP-E-N Wall Mount Transmitter offers reliable and precise measurement of humidity, temperature, and dew point. Designed for long-term stability, it uses a capacitive polymer sensor that resists contamination from dust, chemicals, and moisture, making it ideal for demanding healthcare environments. Its robust output options, including BACnet and Modbus® protocols, allow for seamless integration with centralized building automation systems. By providing real-time data and supporting automated environmental controls, the RHP-E-N helps facilities maintain optimal humidity levels, reduce the risk of airborne disease transmission, and support compliance with ventilation standards in critical care spaces.
To support precise temperature control in hospital HVAC and building automation systems, the TE Duct and Immersion Temperature Sensor offers reliable monitoring for both air and water applications. With a versatile design available in duct mount, immersion, and strap-on configurations, these sensors can be deployed throughout a healthcare facility to capture accurate thermal data from ventilation ducts and water loops. This information feeds into centralized IAQ monitoring systems, helping to ensure thermal consistency in patient rooms, surgical suites, and clean zones.
The CDTV CO₂/VOC Transmitter adds an important layer to hospital IAQ monitoring by combining carbon dioxide and volatile organic compound (VOC) sensing in a single compact unit. This dual-sensor approach enables more responsive and efficient ventilation control by detecting both occupancy levels and harmful airborne contaminants often associated with cleaning agents, off-gassing, or medical equipment. Designed to optimize HVAC operation, the CDTV helps reduce energy costs while maintaining safe air quality thresholds in sensitive environments such as patient rooms, waiting areas, and surgical prep zones.
Building Energy Efficiency
Maintaining energy efficiency in a hospital both reduces operating costs and imporves HVAC system reliability. Differential Pressure Sensors and Occupancy Sensors play key roles in optimizing HVAC performance by monitoring and controlling airflow across filters in air handling units. When pressure drops across a filter, it typically signals restricted airflow caused by particulate buildup. Left unaddressed, this forces fans and blowers to work harder, increasing energy consumption and accelerating equipment wear. Continuously measuring these pressure changes and replacing filters when appropriate ensures systems run at peak efficiency.
The MSX-Pro Magnesense® Differential Pressure Transmitter is engineered for high-accuracy measurement of pressure drop across air filters, making it an essential tool for improving HVAC efficiency in hospital environments. With 32 field-selectable ranges and NIST traceability options, it provides reliable data to detect airflow restrictions caused by filter loading. As filters become clogged, the MSX Pro signals rising differential pressure, prompting timely maintenance before energy waste or IAQ degradation occurs.
The Model-OSC-200 Omnidirectional HVAC Occupancy Sensor enhances HVAC energy efficiency by ensuring that conditioned air is only delivered when spaces are in use. Designed for ceiling mounting with 360° infrared detection, it identifies human presence in a room and can trigger ventilation, lighting, or climate control systems accordingly. By minimizing unnecessary airflow in unoccupied areas (such as administrative offices, storage rooms, or conference spaces), this sensor helps reduce energy consumption without compromising occupant comfort.
Underground Parking Garage
Underground parking structures in hospitals require continuous air quality monitoring to protect occupants from harmful gas buildup. Carbon monoxide (CO) and nitrogen dioxide (NO₂)—which are the emissions from idling or moving vehicles—can accumulate quickly in enclosed areas, posing serious health risks. To address this, hospitals use Gas Transmitters that track pollutant concentrations in real time and trigger ventilation fans only when thresholds are exceeded. This on-demand exhaust control helps reduce energy consumption while maintaining safe air quality standards and supports sustainability initiatives by lowering the building’s overall carbon footprint.
Both the Series GSTC CO/NO2 Gas Transmitter for Garages and Series GSTA CO & NO2 Transmitters for Parking & Docks are purpose-built for monitoring carbon monoxide (CO) and nitrogen dioxide (NO₂) levels in enclosed parking areas such as hospital garages and loading docks. The GSTC features BACnet and Modbus® communication, making it ideal for integration into automated building systems, while the GSTA offers field-selectable analog outputs for flexible control schemes. Both models help optimize fan operation by activating ventilation only when gas concentrations exceed safe limits, which reduces energy usage without compromising occupant safety. With options for electrochemical sensing, field calibration, and robust enclosure designs, these transmitters enable continuous, code-compliant air quality management in high-risk vehicular environments.
Stairwell Pressurization
In healthcare facilities, maintaining clear and breathable stairwells during an emergency is vital for safe evacuation. Stairwell pressurization systems work by introducing clean outdoor air into the stairwell to create positive pressure, preventing smoke from seeping in. This ensures a safe egress path for occupants and emergency responders.
However, running pressurization fans continuously can lead to energy waste and potential overpressurization, making fire exit doors difficult to open. Instead, these systems are typically triggered by a fire alarm signal, which activates both the ventilation fan and a Differential Pressure Transmitter. The fan supplies fresh air, while the transmitter monitors pressure levels within the stairwell. If the pressure exceeds safe thresholds, the system signals a damper to modulate airflow and maintain balance. By coordinating airflow, pressure, and system response in real time, these components ensure the stairwell remains clear of smoke and easily accessible during emergencies—without compromising energy efficiency during normal operation.
The MSX Magnesense® Differential Pressure Transmitter is ideally suited for stairwell pressurization control, providing precise measurement of low differential pressure to ensure safe and balanced airflow. With 32 field-selectable ranges and dual analog outputs, it can simultaneously monitor pressure and temperature or airflow, allowing for fine-tuned control of damper positions during emergency ventilation events. When connected to a building's fire alarm system, the MSX activates alongside the stairwell fan, continuously relaying real-time pressure data to maintain optimal positive pressure—high enough to keep smoke out, but not so high that it prevents exit doors from opening. Its accuracy, flexibility, and ease of integration make it a critical component for life safety systems in hospital environments.
Air Balancing
Proper air balancing in any healthcare environment is critical to maintaining healthy indoor air quality and meeting required air change per hour (ACH) rates. Using an Air Flow Hood can ensure that every room receives the correct amount of ventilation. Maintaining correct airflow balance not only supports infection control efforts but also prevents airborne contaminants from recirculating through the HVAC system or migrating between spaces within the hospital.
The SAH SMART AIR HOOD® is specifically designed to simplify airflow balancing in complex environments like hospitals. Its lightweight construction and ergonomic design allow it to be easily positioned around obstructions such as medical equipment, shelving, and patient beds. To address the unique challenges of healthcare HVAC systems, the SMART Air Hood® is offered with skirt adapter hoods that accommodate oversized or elongated diffusers commonly found in medical facilities.
1 According to the CDC, maintaining negative or positive pressure in specific rooms helps prevent the spread of airborne contaminants.
Source: CDC Guidelines on Environmental Infection Control.
↩
Connect with a DwyerOmega Expert Today!










